What is a Root Canal?
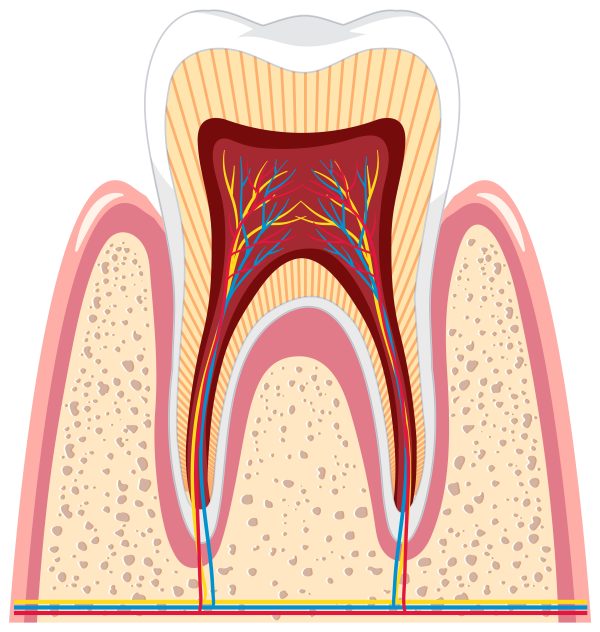
Endodontic treatment, also known as root canal treatment, refers to oral treatments whereby the pulp is cleaned from a tooth, the canals disinfected, cleaned, shaped and filled with a biocompatible material.
Endodontic treatment consists of unroofing the pulp chamber from the top of the tooth and cleaning the chamber and root canal spaces with miniature files. In addition, a cleaning solvent is used to help the disinfection process. Subsequently, the root canal spaces are filled with a plasticized/rubber material. The intention of using files to clean out the canals along with the use of a cleaning solution is to render the tooth lifeless (so it feels no sensation) to alleviate any symptoms of pain.
Each individual tooth is unique in its root and canal configuration and the paths the canals take to the apex (end) of the tooth. Additionally, these canals are not always fully patent and may be calcified. For this reason, the predictable outcome for endodontic treatment is variable depending on each individual case.
Root Canal Process
A tooth is generally assessed to require root canal treatment when a patient feels painful sensations and moderate to severe sensitivity to hot and cold. After a complete endodontic assessment (percussion, bite, cold testing), it will be decided whether root canal treatment is necessary. Additional treatment options may include no treatment, waiting for the development of symptoms or tooth extraction.
Root canal treatment may take from one to several appointments depending on the difficulty and complexity of the case. Once treatment has begun, it is absolutely necessary that the treatment be completed and that the patient follow all prescribed instructions.
During treatment it is important that the treatment area is kept isolated and dry. In order to achieve a clear treatment area, two isolation apparatuses may be used. The first is a Dry-Shield apparatus which is a rubber shield with a bite block that curves around your teeth and rests in your inner cheek and is attached to a vacuum suction. The second is a rubber dam, which places a clamp on your tooth on the side of treatment and a rubber sheet placed around each individual teeth and anchored by the clamp and a metal frame. Local anesthetic will be administered prior to the placement of the isolation device.
The tooth is accessed from the top surface with any caries removed from the entrance of the pulp chamber. The pulp chamber is fully unroofed, the canal orifices are found and accessed with miniature files. The lengths of all the canals are determined and a rotary file machine is then used to clean and shape the canals. A cleaning solution is used throughout the process. Once adequately cleaned and shaped, the canals are filled with a plasticized/rubberized material. The canal orifices are then sealed with a composite material. Often, a temporary filling will be placed for 2-4 weeks to assess the degree of success of treatment. If successful, a permanent filling will then be placed.
It is important to be aware that all endodontically treated teeth are recommended to have crowns placed on them because significant tooth structure has been removed, thereby weakening the tooth and causing a high risk of tooth fracture in the future.
Risks & Complications
There is a risk, however minor or infrequent, associated with even the most careful endodontic treatment. The following serves as an explanation of some (but not all) of these possible risks and complications.
During the process of accessing the pulp chamber, finding canal orifices and instrumenting canals, a perforation of the tooth may occur resulting in either extraction of the tooth or compromised prognosis of treatment. In addition, on rare occasions, there may be damage to existing fillings, crowns and bridges.
During instrumentation of the canals, files may separate in the canal. Sometimes, these breakages can be negotiated and the file can be removed or may become incorporated with the filling material. Referral to a specialist (endodontist) may be required.
The success rate of endodontic treatment varies depending on the difficulty of your specific case. Many factors affect success, including general health, the condition of the nerve and root canal(s), bone support around the tooth, the strength of the tooth, and much more. There may be accessory canals that are not reachable and after treatment the tooth may still be sensitive. It is therefore possible that there is a risk of treatment failure.
Root canal treatment can be sensitive both during and after the final treatment. This sensitivity usually resolves itself within a few days to several weeks. One may also experience some swelling, bleeding, partial numbness and a tingling sensation in the lip, tongue, chin, gums, cheek as well as jaw muscle cramps, periodontal disease, nausea, allergic reactions, burning sensation in tissues, delayed healing and sinus perforation. All this may be due to either local anesthesia, the cleaning solution used or treatment. Symptoms are usually transient, however, rarely they may be permanent.
Root canal treatment requires removing a great deal of tooth structure above the gums as well as internally from canals within the roots. This causes the tooth to be weakened. Additionally, without a blood supply, the tooth loses its vitality and becomes brittle. It is therefore highly recommended that endodontically treated teeth be crowned soon after completion of the treatment. There is a risk of tooth fracture during teeth grinding, improper biting and trauma. Tooth fracture may result in the necessity of extracting the tooth.
Retreatment of root canals may be necessary if symptoms persist or begin again at a later date. Failure of treatment may be due to accessory canals, leakage of restoration, inadequate instrumentation of canals or additional canal configurations. Retreatment may need to be done by an endodontist.

